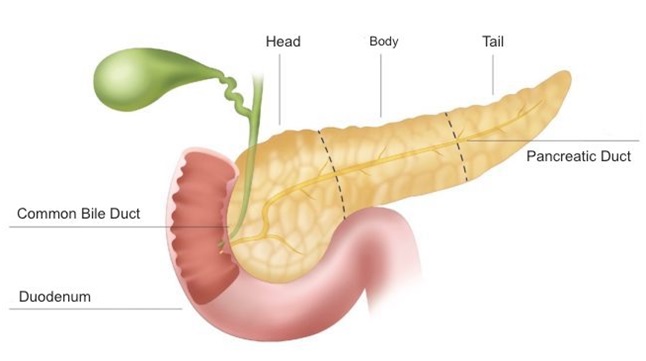
The pancreas has two different secretory tissues, endocrine and exocrine. Endocrine tissue secretes the hormone insulin, which balances blood sugar, and sends it to the body through the blood circulation. Exocrine tissue secretes enzymes necessary for the digestion of fats, carbohydrates and proteins. These enzymes are transported to the duodenum to become active. In some cases, the tissues in the pancreas are damaged in such a way that they cannot do their job. In such cases, various pancreatic diseases may occur due to endocrine and exocrine tissue damage.
The pancreas extends from the liver on the right in the mid-posterior part of the abdomen to the area where the spleen is located on the left side, under the rib arch. It is attached to the duodenum above the horizontal part of the large intestine just behind the stomach. It balances the blood sugar level with the hormones and enzymes it secretes and helps the stomach to digest food. Enzymes produced in the exocrine tissue of the pancreas are effective in the separation of vitamins, minerals, proteins, fats, carbohydrates in the foods we consume and their storage in the necessary parts of the body. its production. The hormone insulin is produced by the endocrine tissue of the pancreas. The hormone insulin helps the body use the nutrients digested by the enzymes secreted by the exocrine tissue of the pancreas.
In Which Situations Do Pancreatic Diseases Occur?
Pancreatic diseases are caused by the inability of the pancreas to balance the "insulin resistance", which has an effect on the normal functioning of the body, and its inability to fulfill its digestive function. The foods we consume must be broken down so that they can be mixed with the blood in order to be processed in the body and ready for use by the metabolism. The pancreas undertakes this task in the body with the enzymes it sends to the small intestine. In some cases, the pancreas is unable to secrete these enzymes. As a result, nutrients are stored in the intestine without being broken down into their parts. This situation leads to the emergence of various diseases that disturb people. Hormones secreted by the pancreas are essential for energy production. However, in some diseases, the pancreas cannot produce enough insulin to balance blood sugar. It becomes difficult for the hormone to mix with the blood, and as a result, the necessary energy for the correct functioning of the metabolism cannot be produced. This situation causes various symptoms related to various pancreatic diseases. Pancreatic diseases may start to show symptoms over time or suddenly. Severe abdominal pain and accompanying symptoms such as vomiting and diarrhea may indicate pancreatic disease. In order to determine whether these symptoms are caused by pancreatic diseases, the patient should be evaluated in detail by an internal medicine specialist and then the preliminary diagnosis made with various tests should be supported.
How Are Pancreatic Diseases Diagnosed?
In order to diagnose pancreatic disease, first of all, it is necessary to learn the patient's history of the disease and the patient's complaints, preferably by an internal medicine specialist, to evaluate the patient by performing a detailed physical examination, and then to use blood tests and appropriate imaging methods to find the exact source of the observed symptoms. If it is thought that there is a problem due to the structure of the pancreas, imaging methods are used. Pancreas and pancreatic ducts can be viewed with various imaging devices such as ultrasonography (USG), magnetic resonance (MR) imaging and computerized tomography (CT). Pancreatic diseases vary considerably in treatment and recovery processes according to their types.
Types of Pancreatic Diseases
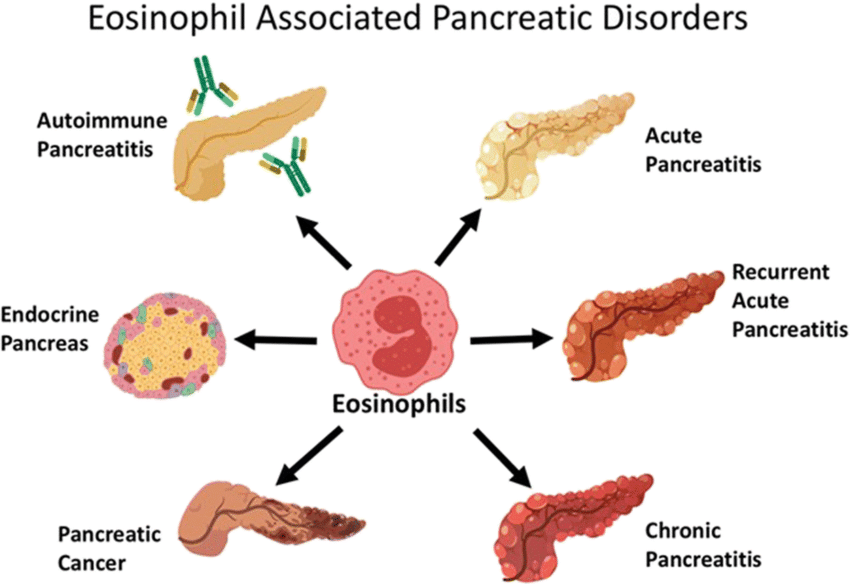
Pancreatic diseases vary according to when the problem in the pancreas starts, whether it is long-term or not, and its symptoms. Acute pancreatitis, chronic pancreatitis, hereditary pancreatitis and pancreatic cancer are types of pancreatic diseases.
Acute Pancreatitis Disease and Causes
Acute pancreatitis is a pancreatic disease with a rapid onset and severe course. Enzymes secreted by exocrine tissues must be delivered to the intestines through the pancreatic ducts in order to perform the digestive process. However, for various reasons, these enzymes remain in the pancreas and cannot pass into the intestines. One of these reasons is gallstones, which cause obstruction in the gallbladder and ducts. Enzymes, due to their nature, should decompose the nutrients in the intestine, but since they cannot reach the intestines, they attack the pancreatic cells and begin to decompose them. These enzymes stored in the pancreas damage the pancreas and create the symptoms of acute pancreatitis seen in the form of attacks in the patient.
What Are the Symptoms of Acute Pancreatitis?
In imaging and blood tests performed on the pancreas, damaged structures in some cells in the pancreas of people diagnosed with acute pancreatitis (pancreatic infection) and blockages in the pancreatic duct can be seen. People with acute pancreatitis symptoms usually:
Severe abdominal pain that occurs suddenly in the lower part of the rib arch where the pancreas is located,
Abdominal pain that comes in the form of pains and spreads to the back and waist in the form of a belt,
Fire,
Complaints such as stomach pain and nausea attacks are seen.
One or more of these symptoms may occur at the same time. Treatment should be started early to correct the damage to the pancreatic tissue.
Can Acute Pancreatitis Be Treated?
The treatment plan is based on controlling the symptoms of acute pancreatitis in the patient, finding the source of the disease causing pancreatitis and treating it. In cases where the source of the problem causing the disease is eliminated, the recurrence of acute pancreatitis in the form of attacks is prevented. The patient can quickly return to his normal life by cleaning the canal section that allows the enzymes secreted from the pancreas to reach the intestine. For this reason, when symptoms such as severe abdominal pain and vomiting are observed, it is necessary to apply to the hospital without delay. It is important to diagnose and treat the disease as soon as it shows symptoms. In the treatment of advanced acute pancreatitis, even if the duct obstruction is removed, it should be kept in mind that the treatment of the disease may spread for a very long time. In cases where the enzymes secreted from the pancreas cannot flow easily into the intestine, oral feeding of the patient is stopped in order to reduce the amount of enzymes secreted from the pancreas and thus to prevent tissue damage. Nutrition is carried out through the vein. Thus, the damaged pancreas is “rested” and the progression of the damage is prevented. Not every pancreatic disease may be a short-term and sudden-onset disease like acute pancreatitis. For this reason, it should be investigated whether the pancreas disease in the person is chronic or not.
Chronic Pancreatitis Disease and Causes
As the damaged cells continue to increase due to recurrent inflammation in the pancreas, permanent damage to the pancreas occurs. This condition is called chronic pancreatitis. It is not a sudden health problem. It develops due to the inability of the pancreas to perform its function over time and the permanent damage it creates in its own structure with the enzymes it secretes. Regular and high alcohol consumption paves the way for the formation of chronic pancreatitis. Chronic pancreatitis can cause other conditions, such as pancreatic insufficiency, as damage to the pancreas progresses.
What Are the Symptoms of Chronic Pancreatitis?
Symptoms of chronic pancreatitis are similar to those of acute pancreatitis. Obstruction of the pancreatic ducts, which causes chronic disease, puts pressure on the pancreatic duct and tissue. Prolonged suppression of the pancreas causes severe abdominal pain. It becomes more and more difficult to stop these pains with painkillers. Since foods cannot be digested in the intestine with pancreatic secretions, indigestion problems, rapid weight loss and diarrhea are common chronic pancreatitis symptoms. In untreated cases, diabetes can occur.
Can Chronic Pancreatitis Be Treated?
Since pancreatic infections mostly occur as a result of obstruction of the common part of the bile duct and pancreatic duct, cleaning this area with endoscopic methods is a candidate to be the most effective treatment if technically possible. starts. Vitamin supplements are also used in the treatment of chronic pancreatitis, as the A, D, E, K vitamins stored in the body contribute to the healing processes of pancreatic patients. Various surgeries may be considered in patients who do not respond to these treatments. Some factors affecting the structure of the pancreas may also cause pancreatic disease. Most of the structural problems can be passed on genetically from generation to generation.
Hereditary Pancreatitis and Its Causes
All the data obtained in the evaluation of patients with pancreatitis show that the cause of many pancreatic diseases may be hereditary. This disease, which is passed on from the family through genes, is a long-term disease similar to chronic pancreatitis. It refers to congenital functional disorders in the structure of the pancreas.
What Are the Symptoms of Hereditary Pancreatitis?
Hereditary pancreatitis does not occur as a result of certain factors such as acute and chronic pancreatitis triggering the pancreas. It is a congenital disease. Symptoms begin to appear with age.
Can Hereditary Pancreatitis Be Treated?
People with a family history of pancreatitis and recurrent episodes of acute pancreatitis are given blood tests and genetic tests. As a result of the tests, treatments are applied to control the pain. These people have a higher risk of developing pancreatic cancer than other members of the community.
Autoimmune Pancreatitis
The effect of the body's immune system attacking its own tissues is referred to as "autoimmune". If the attacked tissue is the pancreas, the resulting disease is called autoimmune pancreatitis. The signs and symptoms of this disease group can mimic acute and chronic pancreatitis as well as pancreatic cancer. Even this group of diseases once again reveals the importance of hepatobiliary disease units in the diagnosis of pancreatic diseases.
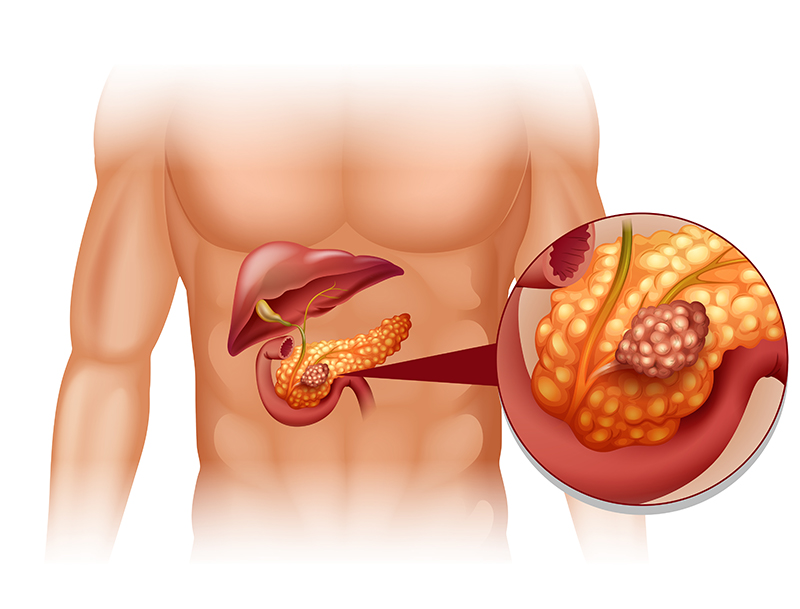
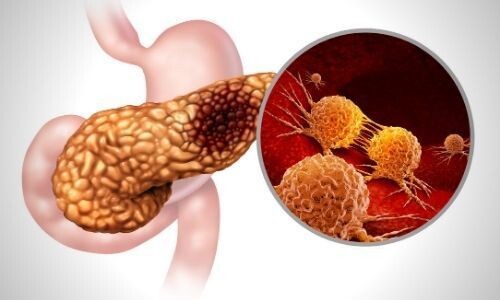
Pancreatic Cancer and Causes
Pancreatic cancer occurs when malignant tumor cells appear and multiply in the pancreas. The causes of the appearance of tumors include hereditary predisposition, chronic pancreatic diseases, obesity and smoking. Malignant tumors arise from the tissue of the pancreas itself. Pancreatic cancer begins to show symptoms in different periods depending on the location of the tumor in the organ.
What are the Symptoms of Pancreatic Cancer?
The symptoms of pancreatic cancer include jaundice, abdominal swelling, severe weight loss in a short time, severe fatigue, and sometimes obvious and sometimes unclear findings. Another important symptom is the sudden onset of diabetes, although there is no hereditary factor. It is suspected that there may be a disease in the pancreas of the person who is admitted to the hospital with the complaint of diabetes that suddenly appears. With the help of imaging devices such as USG, CT and MRI, a malignant tumor in the pancreas can be diagnosed by a radiologist. In addition, it should not be forgotten that the symptoms of pancreatic cancer usually begin to appear in the advanced period. In advanced cancer cases, it becomes much more difficult to control the tumor. For this reason, it is vital to start the treatment without delay in pancreatic cancer diagnosed.
Can Pancreatic Cancer Be Treated?
As in other cancers, the planning of pancreatic cancer treatment begins by determining the size of the tumor in the organ, whether it has spread to neighboring tissues, and whether it has spread to other organs. If the tumor has not technically exceeded the operable limits and is at an appropriate stage, it should be surgically removed. Surgery is planned according to the location of the tumor in the pancreas. While Whipple surgery (pancreaticoduodenectomy surgery) is applied to pancreatic tumor located in the pancreatic head and uncinate process of the pancreas, distal pancreatectomy and splenectomy (removal of the spleen) surgery is performed for tumors located in the body and tail of the pancreas. Performing the surgery with any of the open, laparoscopic or robotic methods has no difference in terms of the expected life expectancy of the patient after the surgery. The important thing is the appropriate surgical intervention without compromising the principles of cancer surgery, in which the surrounding lymph nodes are removed without leaving any tumor behind. This should be shaped according to the preference of the Hepatopancreatobiliary (HPB) Surgical team and ultimately the acceptance of the patient and their relatives. If the malignant tumor has spread to vital structures such as adjacent main vessels, has spread widely to other distant organs or to the abdomen, surgical removal of the tumor is not an appropriate approach, as it will not help prolong the life expectancy of the patient, even if it is technically possible. For patients at this stage, non-surgical alternative treatment methods such as chemotherapy and radiotherapy should be applied.