









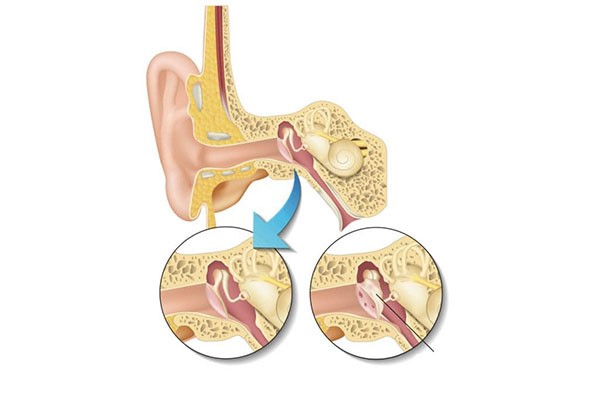
"Tympanoplasty" surgery, which is applied in eardrum perforations and chronic middle ear diseases, is technically the repair of the eardrum and the auditory system in the middle ear, as well as the cleaning of the inflammation in the middle ear and the mastoid bone behind the ear.
Depending on the extent of the existing disease, the operation can be performed as only repairing the hole in the eardrum (myringoplasty), repairing the ossicular system providing sound transmission in the middle ear with membrane repair (tympanoplasty), clearing the inflammation that has progressed into the mastoid bone (mastoidectomy) or a combination of these operations (tympanomastoidectomy).
When is Tympanoplasty Surgery Performed?
In patients who have a hole in the eardrum but do not have a significant hearing loss and there is no discharge unless water escapes into the ear, the surgery to be performed to close this hole is generally aimed at increasing the patient's quality of life and preventing the progression of hearing loss over time by eliminating the need to protect the ear from water during bathing and swimming. performed according to the patient's preference.
Although the patient's ear is protected from water and there is no inflammatory focus in the nose and sinus region that will cause ear discharge, if recurrent ear discharges are observed, the hole in the membrane should be closed in order to improve the quality of life and to prevent the progression of hearing loss or serious problems related to inflammation. In these patients, both the hole in the membrane is closed and the problems in the small middle ear ossicles that transmit sound are intervened during the same surgery.
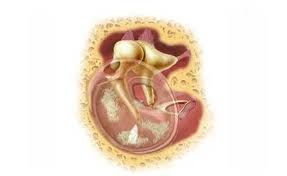
If an inflamed tissue called cholesteatoma is detected in the middle ear and mastoid bone, which progresses by dissolving the bone, this inflammation should be removed with surgery as soon as possible. In patients with cholesteatoma, the protection or repair of the hearing system is the second priority, and the main purpose is to clear the inflammation before it causes facial paralysis, inner ear-related hearing loss or intracranial complications (meningitis, brain abscess, etc.).
Surgery Technique
While deciding on the technique of the surgery, the condition of the disease, the location of the hole on the membrane, the structure of the ear canal, whether to intervene in the mastoid bone behind the ear during the operation, the preferences of the surgeon and finally the patient are effective.
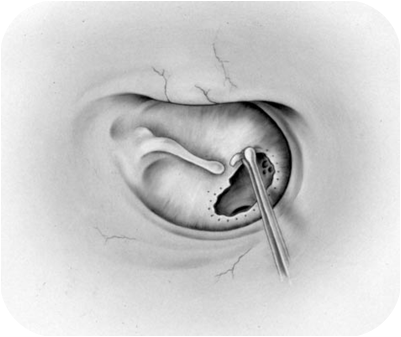
Although very different surgical techniques are applied under the microscope in the middle ear and mastoid bone during the surgery, questions are frequently asked about this subject, since the patient and their relatives can see the surgery because it is limited to the incision in the skin.
Tympanoplasty surgery can be performed through incisions made through the ear canal, inside the ear or behind the ear. While surgery can be performed through the ear canal without an additional incision to repair only a small hole in the membrane, the approach applied by making an incision behind the ear is preferred in the holes in the middle and back of the membrane, through the ear, in the holes in the anterior part of the membrane and in cases where intervention is required to the mastoid bone. The main deciding factor in this regard is the preference of the surgeon who will perform the surgery.
The most commonly used tissue for the repair of the eardrum is the temporal muscle sheath. Since this tissue is close to the surgical site, it can be easily obtained during surgery. The cartilage membrane in front of the ear canal or ready-made materials (such as sterile meninges pieces that have undergone appropriate processing) can also be used. In recent years, repair (cartilage tympanoplasty) using thin cartilage strips obtained from the cartilage in front of the ear canal, especially in large holes, has started to be preferred more and more due to both the ease of application and the success of the results.
When a repair is required to ensure the transmission of sound due to damage to the ossicles that conduct hearing, many different materials such as prostheses made of various materials, parts obtained from the cartilage in front of the ear canal, and the middle ear ossicles can be used by positioning and shaping.
Postoperative
Patients can usually be discharged from the hospital by dressing them on the first day after surgery.
Special sponges in the external ear canal are cleaned at the end of 10-14 days in surgeries that do not involve intervention on the mastoid bone, and it is recommended that patients protect their ears from water and use ear drops containing antibiotics and cortisone in order to prevent infections and reactions in the operation area. Recovery in this group is completed in 3-4 weeks. In general, in the first month, it is necessary to be protected from flu infections and blows, and not to travel by plane. In these patients, the technical and functional success rate of the surgery is generally quite good, depending on the extent of the pathology and the preoperative hearing level.
In patients who have undergone intervention to the mastoid bone during the surgery, various dressings should be applied for varying durations depending on the type of surgery performed. Healing takes longer in this group, and the hearing gain in these patients is generally less than in the other group.
Especially if the cholesteatoma is located in the vicinity of the facial nerve and inner ear, the bone cannot be scraped in these areas in order not to damage the nerve and hearing, and disease may remain at the cellular level.
Since the risk of recurrence of cholesteatoma is high in these patients, follow-up examinations should be performed at regular intervals after surgery. In this group of patients, interventions for the restoration of the auditory conduction system can be performed when the cholesteatoma recurs in small foci or in the second-look control surgery to be performed 6-12 months later.
As a result, there is no standard approach for tympanoplasty surgeries that will suit every patient. In the selection of surgical techniques and applications to be used during the operation, especially in cases with cholesteatoma, the characteristics of the disease and the patient, the factors determined during the surgery and the surgeon's experience are effective.