
Colon and rectum are part of the digestive system. The large intestine is the organ that comes after the small intestine and has an average length of 1.5 m. It starts with the caecum from the lower right side of the abdomen in the form of an inverted U letter, goes up and turns under the liver and passes the abdomen horizontally. It comes under the spleen located in the upper left corner and again makes a turn and moves downwards from the left side and merges with the rectum. The rectum is the last part of the digestive system, with an average length of 15 cm and formed as a result of the enlargement of the large intestine.F
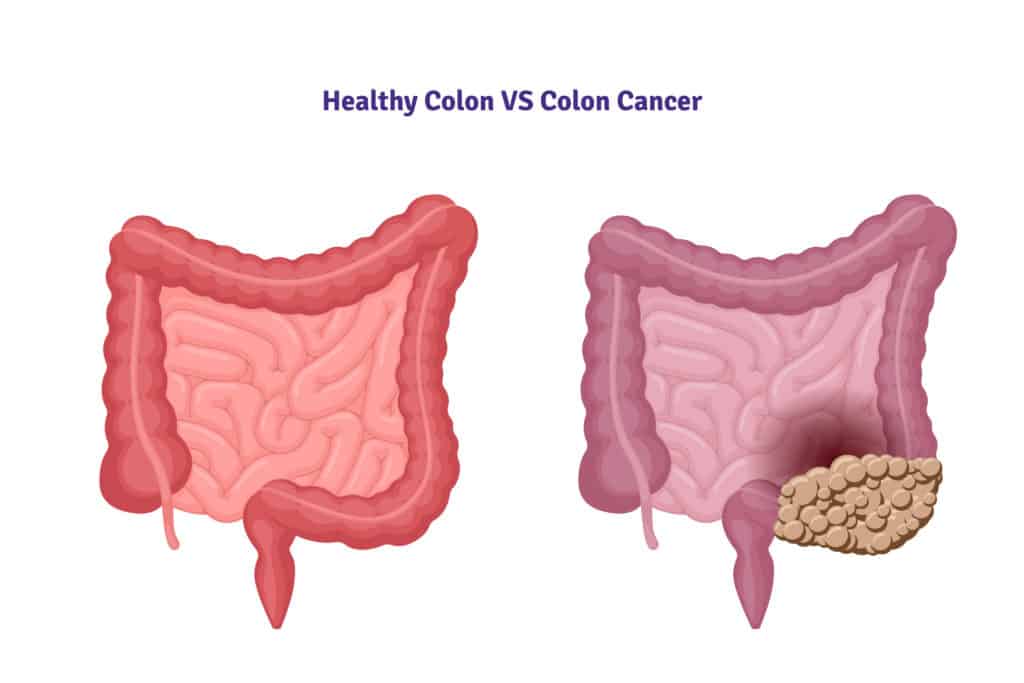
Colon cancer starts in cells in the colon. As the number of cells increases, it spreads around the column in a circular fashion like a napkin ring. If diagnosed early, cancer cells can only be detected within the colon. If not diagnosed early, cancer may spread to nearby organs, lymph nodes, and through the bloodstream to the liver, lungs and other organs.
The most important criterion for success in colon cancer treatment is early diagnosis. When colon or large intestine cancer is detected at an early stage, it is possible to completely get rid of the disease.
In developed countries, the rate of colon and rectal cancer is 4 to 10 times higher than in developing countries. Causes of colorectal cancer; lifestyle, changes in environmental factors and hereditary genetic factors.
Genetic Factors
A person with a family history of colorectal cancer has a higher risk of cancer. Inherited genetic factors increase the risk ratio. Both familial adenomatous polyps in the large intestine and hereditary nonpolyp colorectal cancer, also known as Lynch syndrome, increase the risk of colon cancer. Although genetic colorectal cancers constitute only 5-10% of the disease, people with these genetic factors are younger than other colon cancer patients and carry a higher vital risk.
Hereditary nonpolyposis colorectal cancer (Lynch Syndrome) is the most common of the genetic colorectal cancers. It occurs as a result of incompatible DNA pairings, with inherited gene mutations. The average age at diagnosis is 45. This type of gene mutation predisposes to the formation of cancer of the endometrium (inner lining of the uterus), ovary, small intestine, ureter (urinary tract), and renal pelvis (kidney pool).
The presence of cancer in the family and first degree relatives of the person seriously affects the emergence of the disease. People with a family history of colon cancer should start having a colonoscopy 10 years before, at what age their relative was diagnosed with colon cancer. Completely healthy people who do not have a family history of colon cancer or have no complaints should have a colonoscopy at least once from the age of 50.
Can Polyps Cause Colon Cancer
In the formation of colon cancer; In addition to excessive fat, red meat-based diet, obesity, smoking and alcohol consumption, polyps are effective. When polyps are seen in the large intestine during screening colonoscopies, it is possible to prevent the disease by removing them before they become cancerous. Having a history of breast and ovarian cancer in women also increases the risk of colon cancer in these people. It is recommended that people with breast and ovarian cancer be screened for colon cancer before the age of 50.
Polyps usually begin to show symptoms in the late period, that is, when they turn into cancer. Only a small percentage of polyps turn into cancer. However, since the majority of cancers develop from polyps, it is an issue that needs attention. When we look at the general population, this rate is around 10-15%. Different types of polyps are seen in approximately 25% of the population around the age of 50. When we evaluate the age of 70, the incidence is close to 50%; that is, the incidence of polyps increases with age.
Features of polyps;
It doesn't go away on its own.
It has genetic features. Patients with first-degree relatives with colon cancer and polyps in previous examinations constitute the risk group and need close follow-up.
Polyps are usually around 1 cm. Larger than 2 cm can be dangerous and must be removed.
Symptoms such as severe pain, intestinal obstruction, weight loss are usually late symptoms. Problems such as hemorrhoids and fissures in the anus may cause delays in the diagnosis and treatment of rectal cancer in some patients because they have similar symptoms. These symptoms can mislead both patients and, rarely, physicians. In general, the possibility of rectal and large intestine cancer should be well investigated in bleeding from the breech region over the age of 40.
It is not yet possible to prevent the formation of polyps. Those who have adopted a sedentary lifestyle, people with extreme stress, those who use cigarettes and alcohol, those who are obese, and those who eat predominantly red meat are at risk. However, eating pulpy foods, not smoking, that is, anything that regulates bowel movements is an important factor in preventing the formation of polyps.
Other Colon (Large Intestine Cancer) Risk Factors
Age: Although it can occur at any age, it is mostly seen in people over the age of 50. The risk of colon cancer increases with age. The rate of developing colon and rectum cancers in patients over 60 years of age is 10 times higher than those under 40 years of age.
Intestinal Inflammations: There are basically two types of intestinal inflammation. First; It is ulcerative colitis, that is, ulcerative colitis that occurs in the colon mucosa due to infection. The second is Crohn's disease, which occurs with intermittent inflammation in any part of the digestive system from the mouth to the anus, or in several different parts at the same time. Although it is a long-lasting and chronic disease, it can be treated. Because of the high risk of cancer, colorectal cancer screening tests should be done more frequently.
Nutrition: The incidence of colon and rectal cancers is quite high, especially in the USA and European countries where fast food consumption is common. Consumption of pulp-free food increases constipation, causing stool to remain in the intestine for a long time and cancer of that area. Delicatessen products, pickles, smoked meats, barbecue type foods and fried foods are constipating foods. In addition, it has been determined that consuming foods rich in fruits, vegetables, legumes, chicken and cereals reduces the risk rate.
Obesity: Excess weight increases the risk of colon cancer, regardless of whether it is a woman or a man.
Smoking: Many studies have stated that there is a relationship between cigarette consumption and colon cancer.
WHAT ARE COLON CANCER TREATMENT METHODS?
In colon cancer, surgery may not be required when the cancer is detected at an early stage on polyps taken in colonoscopy. Only closely followed. Colonoscopy is of great importance in the diagnosis of polyps at an early stage, before they turn into cancer. Studies conducted in recent years have shown that colon cancer can be largely prevented by early removal of polyps by performing colonoscopy. For this reason, every man after the age of 45 and every woman after the age of 50 should have a stool screening for occult blood and a colonoscopy. Patient comfort is given great importance during colonoscopy. For this reason, the patient is made semi-conscious with a mild pain reliever called "conscious sedation". Beforehand, the intestine must be completely emptied by various methods. Then, the intestine is entered with a fiberoptic camera and all visible polyps are removed. However, the experience of the physician performing the colonoscopy, the disinfection of the device used and the high image quality are of great importance.
The standard treatment option in advanced colon cancer is surgery; In other words, it is the removal of the tumor area with some healthy tissue and lymph nodes from the environment. Studies show that surgery performed by experienced surgeons in accordance with the principles of oncology is the most important factor for the patient's future. After surgery in colon cancer, additional, protective chemotherapy is applied according to the stage of the disease. For example, in “stage III” cases where the tumor has spread to the lymph nodes adjacent to the intestine, “adjuvant” chemotherapy (preventing the spread of the disease) is now a standardized practice all over the world.
In colon cancers, in tumors very close to the anus, it is sometimes unavoidable to cancel the anus and pass from the abdomen to defecation (with colostomy bags). However, in recent years, preoperative chemotherapy with radiotherapy can significantly protect the anus. In patients who have spread to other organs (metastatic), all three treatment methods (surgery, chemotherapy, radiotherapy) are applied depending on the general condition of the patient, age, and extent of the disease. The aim is to increase the life expectancy and quality of patients. Thanks to the new targeted biological drug therapies in the last few years, the success rates in treatment are increasing day by day.
Nutritional styles and screening tests are of great importance in the protection of individuals who have not been diagnosed with colon cancer. It is important to consume plenty of fibrous foods such as vegetables, fruits and cereals, and to get enough calcium and vitamin D. Besides these; Early diagnosis with screening tests as a secondary prevention measure has a special importance. For this, screening tests are recommended for both sexes, starting from the age of 50. In individuals with a family history of colon cancer, screening tests should be started at an earlier age.